
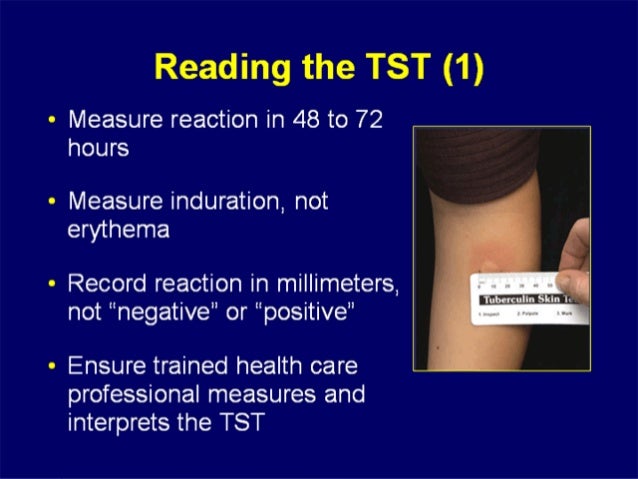
The dosage for PPD-S formulation is five units in 0.1 ml. The dosage of PPD-S and RT-23 formulations differ. Other tuberculin antigens, such as RT-23, are sometimes used outside the United States. In the United States, two US Food and Drug Administration (FDA)-approved PPD tuberculin antigens are available: Tubersol and Aplisol. The PPD test should be read between 48 and 72 hours after administration. It takes approximately six to eight weeks after exposure to bacteria for the PPD test to become positive.

The peak of the induration reaction occurs 24 hours after the test and is secondary to cell infiltration. The test results are interpreted by measuring the delayed-type hypersensitivity reaction. Non-tuberculous mycobacteria are identified by a letter other than S. A standardized PPD-S utilizes a tuberculous mycobacterium. The tuberculin protein used in the test is extracted from Mycobacterium tuberculosis cultures and is used as a purified-protein derivative. In 1934, Florence Seibert published her method of obtaining the purified-protein derivative, effectively creating the PPD test.

Charles Mantoux was credited with creating the technique of injecting material intradermally on the inner surface of the forearm. Robert Koch described the tuberculin reaction in 1890, and Felix Mandel developed the test in 1908. Instead, it is a clinical diagnosis based on a history of prior TB infection and ruling out active disease. There is no definitive test to diagnose LTBI. Therefore, symptom assessment and further testing with chest radiography, sputum test for acid-fast bacilli, or chest computed tomography scans are essential to diagnosing active infection. Notably, a positive test does not distinguish between latent and active TB. Interferon-gamma release assay blood test (IGRA) īoth tests measure delayed-type hypersensitivity reaction or type IV cell-mediated immunity involving T-lymphocytes, which are activated after exposure to mycobacteria. Two screening tests are available to detect TB infection in the United States: The risk of progression in infants is 50%, and this decreases to 1% to 2% by age ten. The risk of LTBI progression to active disease declines with age, secondary to increased immunity. Therefore, detection and treatment of latent TB are critical to controlling the spread of TB and reducing the disease burden. The risk of LTBI progressing to active disease is greatest within the first two years of exposure. Those with immunocompromised states are at an increased risk of reactivation and progression to active TB disease, which is symptomatic and highly contagious. LTBI is asymptomatic and non-infectious.Įarly diagnosis of active TB is crucial to managing and preventing its spread. Ī person with an active infection usually presents with constitutional symptoms, including unexplained weight loss, fever, fatigue, loss of appetite, and night sweats.
tuberculosis. Although the overall incidence and prevalence of tuberculosis have declined, the incidence of multidrug-resistant tuberculosis remains significant. It is estimated that more than 1.7 billion people are infected with M. Treatment for TB is available and effective, yet it remains a significant public health concern and a leading cause of morbidity and mortality worldwide, especially in developing countries. However, it can affect numerous organ systems.

It is a highly contagious droplet infection that primarily affects the lungs. Tuberculosis (TB) is a potentially fatal bacterial infection caused by the bacterium Mycobacterium tuberculosis ( M.


 0 kommentar(er)
0 kommentar(er)
